Sickle Cell Disease (SCD) Program
OVERVIEW
The Sickle Cell Disease (SCD) Program is a specialized initiative dedicated to diagnosing, treating, and managing inherited blood disorders, such as sickle cell disease and thalassemia. This program brings together a multidisciplinary team of experts - hematologists, nurses, social workers, and other healthcare professionals to deliver comprehensive care for individuals affected by these conditions.
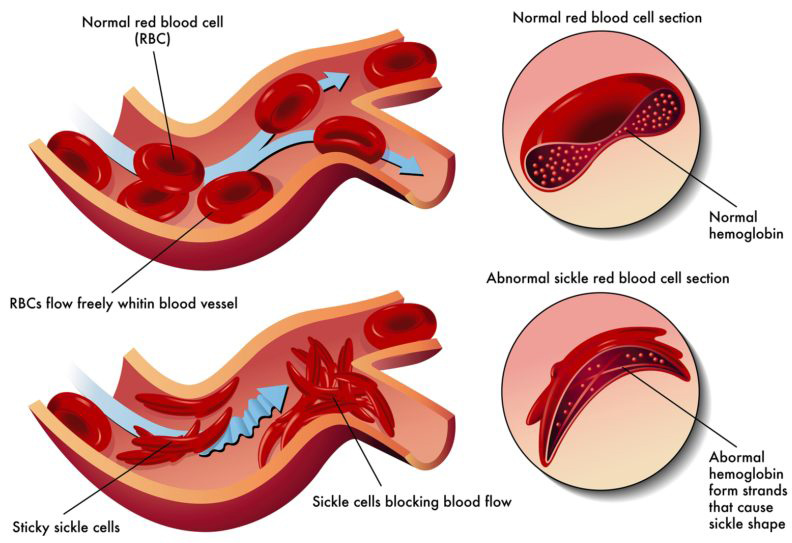
Sickle cell disease is a genetic condition that affects hemoglobin, the protein in red blood cells responsible for transporting oxygen throughout the body. In individuals with this disorder, the body produces an abnormal type of hemoglobin known as hemoglobin S, which causes red blood cells to take on a rigid, sickle-shaped form.
Symptoms of Sickle Cell Disease
The symptoms of sickle cell disease are primarily caused by the sickling of red blood cells. When these cells become sickle-shaped, they break down too quickly, leading to anemia.
Learn More
This can result in shortness of breath, fatigue, and delayed growth and development in children. The rapid destruction of red blood cells can also cause jaundice, which is a yellowing of the skin and eyes. Painful episodes occur when the rigid, sickled red blood cells block small blood vessels, restricting oxygen-rich blood to tissues and organs. This can cause organ damage, particularly in the bones, lungs, kidneys, spleen, and brain.
A serious complication of sickle cell disease is pulmonary hypertension, a condition where blood pressure rises in the vessels supplying the lungs. Pulmonary hypertension affects about one-third of adults with sickle cell disease and can lead to heart failure.
Sickle cell disease (SCD) and sickle cell trait (SCT) are inherited genetic conditions that are passed down from parents to children at the time of conception. These conditions cannot be acquired later in life, nor can they be lost over time. A person born with sickle cell trait or sickle cell disease will always have that condition.
Learn More
- Sickle Cell Trait (SCT):
- A person who inherits one sickle cell gene (hemoglobin S) and one normal gene (hemoglobin A) has sickle cell trait.
- People with sickle cell trait are usually asymptomatic but can pass the sickle cell gene to their children.
- Sickle Cell Disease (SCD):
- A person with sickle cell disease inherits two sickle cell genes (one from each parent).
- This condition can lead to serious health problems like pain crises, anemia, and organ damage.
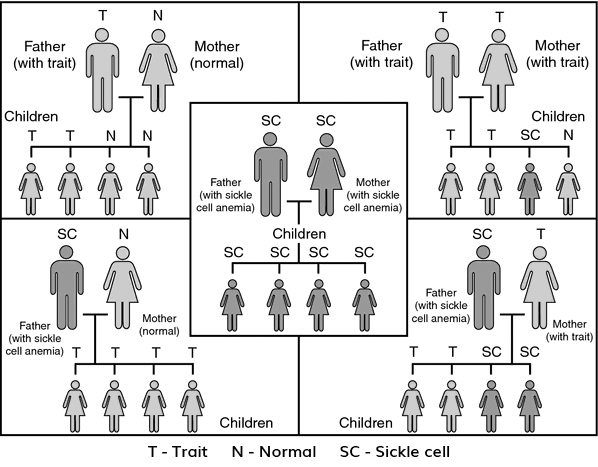
How Inheritance Works
The inheritance of sickle cell follows the principles of autosomal recessive inheritance, which means both parents must carry the sickle cell gene for a child to inherit the disease. Here are the possible gene combinations:
When Both Parents Have Sickle Cell Trait (SCT):
If both parents have sickle cell trait (each with one sickle cell gene and one normal gene), there are four possible genetic combinations for their child:
- 1 in 4 chance (25%) the child inherits two normal genes (normal).
- 1 in 4 chance (25%) the child inherits two sickle cell genes (sickle cell disease).
- 2 in 4 chance (50%) the child inherits one normal gene and one sickle cell gene (sickle cell trait).
When One Parent Has Sickle Cell Trait (SCT) and the Other Parent Has Normal Genes:
If one parent has sickle cell trait and the other is completely normal (not carrying the sickle cell gene), each child has:
- 50% chance of inheriting a normal gene and being normal.
- 50% chance of inheriting one sickle cell gene (sickle cell trait).
In this case, the child can't inherit sickle cell disease because there is no chance of inheriting two sickle cell genes.
Key Points:
- Sickle Cell Trait (SCT) means you carry one sickle cell gene and one normal gene, but usually don't have symptoms.
- Sickle Cell Disease (SCD) means you inherit two sickle cell genes (one from each parent).
- Sickle cell disease or trait is passed from parent to child at conception; it cannot develop later in life.
- Both parents must have the sickle cell gene to pass it on to their child with a chance of having sickle cell disease.
Understanding these inheritance patterns is crucial for individuals with sickle cell trait or disease to make informed decisions about family planning and the potential risks to their children.
Genes Related to Sickle Cell Disease
Sickle cell disease is linked to mutations in the HBB gene, which provides the instructions for making beta-globin, one of the protein subunits of hemoglobin. Hemoglobin is made up of four subunits: two alpha-globin and two beta-globin. The most well-known mutation in the HBB gene causes the production of hemoglobin S (HbS), a defective form of beta-globin.
Learn More
In addition to HbS, mutations in the HBB gene can lead to other forms of abnormal hemoglobin. For example, hemoglobin C (HbC) is another abnormal version of beta-globin, which is more common among people of African descent. In some cases, HBB gene mutations result in low production of beta-globin, a condition known as beta thalassemia.
In individuals with sickle cell disease, both copies of the HBB gene (one from each parent) are mutated, leading to the exclusive production of hemoglobin S. On the other hand, individuals with sickle cell trait carry one normal HBB gene and one mutated one, so they produce a mix of normal hemoglobin (HbA) and hemoglobin S.
Other variations of sickle cell disease occur when one mutated HBB gene produces hemoglobin S, and the other produces a different abnormal hemoglobin. For example, in sickle cell-hemoglobin C (HbSC) disease, people have both hemoglobin S and hemoglobin C in their red blood cells. When hemoglobin S combines with beta thalassemia mutations, the result is hemoglobin S-beta thalassemia (HbSBetaThal).
MEET THE TEAM
Dr. Andrea Cervi
Adult Hematologist
Lori Clarke
Registered Nurse
519-254-5577 x58640
Sydney Galloway
Social Work
Stasha Todorovic
SCAGO Patient Wellbeing Coordinator
Julia Thibert
Social Work
RESOURCES AND INFORMATION
Information for Individuals with Sickle Cell Disease
Information for Healthcare Providers
FAQ's
If you have SCD, please follow the recommendations below:
- If you develop a fever of 38°C (100.4° F): From Monday to Friday (between 8:30 a.m. and 4:00 p.m.), please call the Sickle Cell Disease Nurse immediately. If it is after 4:00 p.m. or on a weekend, please go directly to the Emergency Department.
- If you are experiencing pain: Please follow your current pain plan to manage sickle cell pain at home. If you continue to experience pain, call your Nurse Case Manager immediately from Monday to Friday (between 8:30 a.m. and 4:00 p.m.). If it is after 4:00 p.m. or on a weekend, please go directly to the Emergency Department.
- If you are having difficulty breathing, chest pain or changes in mental status: Go directly to the Emergency Department.
- If you are having a painful erection or a prolonged erection that will not go away (greater than 2 hours): Go directly to the Emergency Department.
- If you are having pain that does not feel like your sickle cell pain: Go directly to the Emergency Department.
- Call ahead and speak to the Charge Nurse: If you are coming to the ER: 519.254.5577, OUE Ext. 34401, MET Ext. 52222.
- When to call 911:
- Severe pain
- Severe headache
- Difficulty speaking or slurring of speech
- Sudden weakness, loss of feeling, or inability to move a body part
- What to bring with you to the emergency department:
- Medications
- Your sickle cell card: If you do not have a card, please request a card at your next clinic visit.
|
SCD Clinic Wallet Card Example
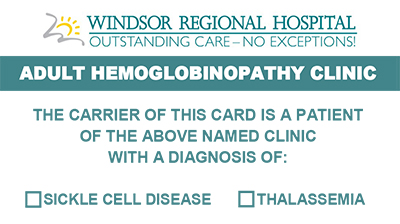
Front
Back
|
The Patient Assistance Fund provides financial support to patients in need, helping to cover healthcare-related expenses such as medications, treatments, and transportation to appointments. If you're struggling with the cost of your care, our clinic can guide you through the application process to see if you're eligible for assistance.
|
|
Our clinic iPads are available for language services, to assist with filling out forms, accessing medical information, and providing educational resources during your visit. The iPads are secure and user-friendly, and our staff will be happy to help you navigate them during your appointment.
|
UPCOMING EVENTS
- SCAGO Holiday Party - December 13, 2025
- Virtual continuing medical education event: Sickle Cell Disease in Practice - Building Awareness & Improving Care. Thursday, November 27, 2025, 5:00-7:30 p.m.
- Pickle for Sickle - a fundraising event to drive the WRH patient assistance fund (details to come!)
PAST EVENTS
- SCAGO Summit, 2025
- Sweet Treats for Sickle Cell Disease - June 26, 2025, WRH, Met Campus
- Regional Education Event on the Care of People with Sickle Cell Disease - June 7, 2025, DoubleTree Hilton.
CONTACT US
Hours of Operation:
Monday to Friday from 8:30 a.m. - 4:00 p.m.
Location:
Windsor Regional Cancer Program
1995 Lens Avenue,
Windsor, ON
N8W 1L9
Phone:
Call Centre: 519-253-5253
Email:
scdteam@wrh.on.ca